Abstract
AbstractBackground: Epstein-Barr virus (EBV) reactivation is one of the most important infections after haploidentical related donor (HID) hematopoietic stem cell transplantation (HSCT). We aimed to establish a comprehensive model with machine learning, which could predict EBV reactivation after HID HSCT with antithymocyte globulin (ATG) for graft-versus-host disease (GVHD) prophylaxis.
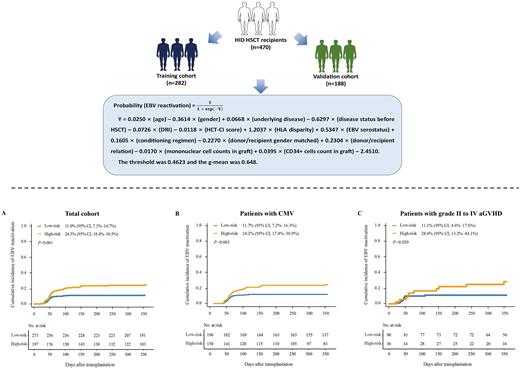
Method: We enrolled 470 consecutive acute leukemia patients, 60% of them (n=282) were randomly selected as training cohort, and the remains 40% (n=188) were used as validation cohort.
Results: The equation was as follows: Probability (EBV reactivation) = , where Y = 0.0250 × (age) - 0.3614 × (gender) + 0.0668 × (underlying disease) - 0.6297 × (disease status before HSCT) - 0.0726 × (DRI) - 0.0118 × (HCT-CI score) + 1.2037 × (HLA disparity) + 0.5347 × (EBV serostatus) + 0.1605 × (conditioning regimen) - 0.2270 × (donor/recipient gender matched) + 0.2304 × (donor/recipient relation) - 0.0170 × (mononuclear cell counts in graft) + 0.0395 × (CD34+ cells count in graft) - 2.4510. The threshold of probability was 0.4623, which separated patients into low- and high-risk groups. The 1-year cumulative incidence of EBV reactivation in the low- and high-risk groups was 11.0% versus 24.5% (P < 0.001), 10.7% versus 19.3% (P = 0.046), and 11.4% versus 31.6% (P = 0.001), respectively, in total, training, and validation cohorts. It also could predict relapse and survival after HID HSCT.
Conclusion: We established a comprehensive model which could predict EBV reactivation in HID HSCT recipients using ATG for GVHD prophylaxis.
Importance:We established a comprehensive model with machine learning in HID HSCT recipients using ATG for graft-versus-host disease prophylaxis, which separated patients into low- and high-risk groups. It could predict EBV reactivation in total, training, and validation cohort. It could predict EBV reactivation in patient with or without CMV infection, and it could also predict EBV reactivation in patients with or without acute GVHD. It could also predict relapse and survival after HID HSCT. This was the first predicted model for these patients who have a high risk of EBV reactivation and it can be popularized easily. It can also help to conduct risk stratification−directed EBV prophylaxis after HID HSCT.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal